No.1 Obstetrics and Gynecology at BL Tiwari Memorial Hospital in Mathura
Dr Varsha Tiwari is the Top Obstetricians & Gynecologists in Mathura for patient care. Dr. Tiwari on her quest for holistic women care across all ages. She works at BL Tiwari Memorial Hospital in Mathura where Dr. Varsha Tiwari is working as a doctor and gynecologist. Prior to this, Dr. Tiwari was an obstetrics and gynecology consultant who specializes in female fitness related disorders. She is a recognised healthcare provider in the area because of her experience for handling obstetrical problems. Dr. Varsha Tiwari is admired for her knowledge and dedication to patient care. Her patients benefit much from her great treatment and counsel on matters related to women’s health.
Obstetrics
General surgery includes a wide range of surgical techniques for the diagnosis and management of illnesses and injuries in any part of the body. Its range of interest includes, among other places, the skin, breasts, belly, peripheral vascular system, and head and neck. As a medical specialty, general surgery focuses on the diagnosis, treatment, and management of a broad range of disorders that affect different body areas. Surgery involving the belly, digestive system, breast, skin, and soft tissues falls within the training of general surgeons.
This specialty may concentrate on the abdominal viscera, which includes the stomach, appendix, spleen, liver, gall bladder, and bile ducts, as well as the small and large intestines. Dr. Brijendra Tiwari is a top general surgeon in Mathura who has expertise in general and laparoscopic surgery.
Gynecologist
Laparoscopic surgery, also known as bandaid surgery, keyhole surgery, or minimally invasive surgery (MIS), is a contemporary surgical technique that allows for smaller incisions (typically 0.5 to 1.5 cm) to be used for abdominal operations as opposed to larger incisions required for traditional surgical procedures. TV monitor images are used during keyhole surgery to magnify the operative parts. While thoracoscopic surgery refers to keyhole surgery done on the thoracic or chest cavity, laparoscopic surgery encompasses operations within the abdominal or pelvic cavities. Endoscopy is a general term that includes procedures like laparoscopic and thoracoscopic surgery. When compared to an open treatment, laparoscopic surgery has several benefits for the patient. These include less bleeding, a quicker healing period, and less pain from fewer incisions.
Services
Prenatal Checkups
Monitoring the health of both mother and baby during pregnancy.

C-Section
Deliver a baby through incisions in the mother’s abdomen and uterus.


MTP Service
Pregnancy termination, ensuring women’s health and well-being.

DNC
Minor surgical procedure involving dilation of the cervix & scraping.
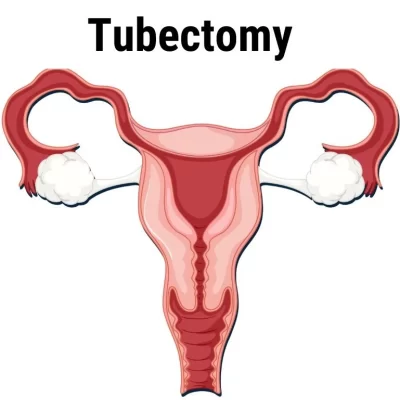
Tubectomy
Female sterilization that involves cutting, to prevent pregnancy.

Polyps
Colon, nasal passages, and uterus, often surgical removal.

High-Risk Pregnancy
Gain potential for complications due to factors like maternal age.

Belly Hysterectomy
Procedure to remove the uterus by incision in lower abdomen.

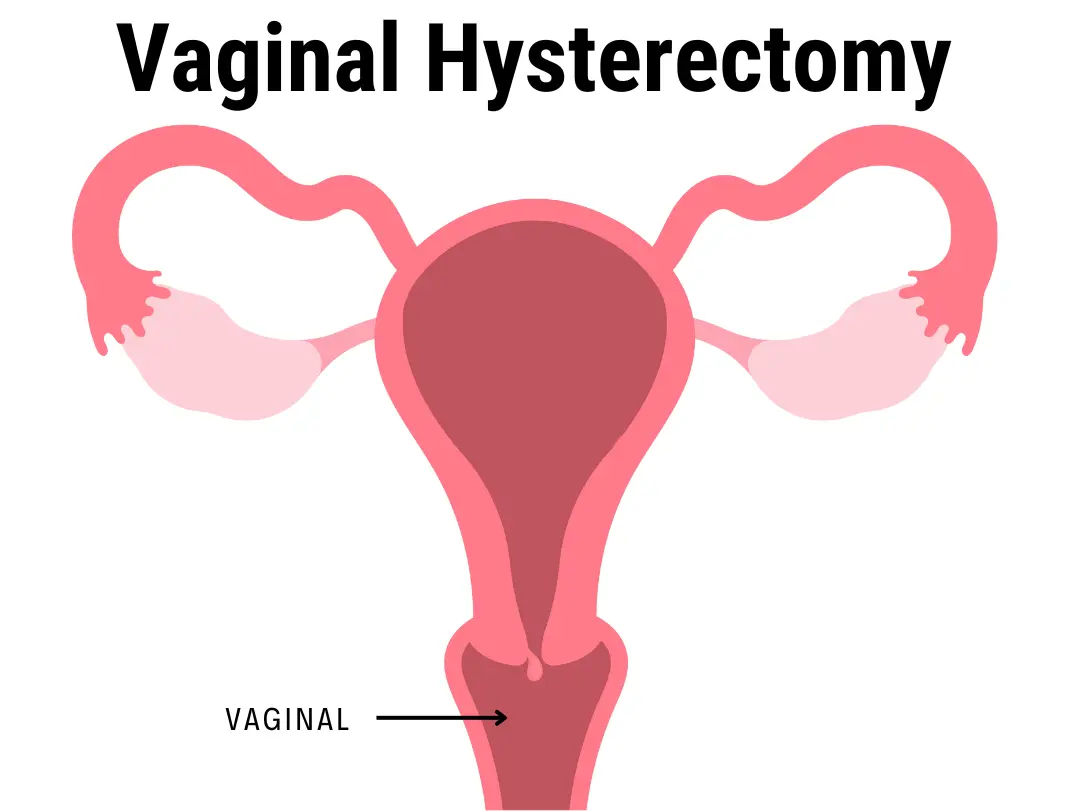
Vaginal Hysterectomy
Remove the uterus through vagina to treat gynecological conditions.

Uterine Fibroids
Non-cancerous growths in the uterus that cause heavy menstrual bleeding

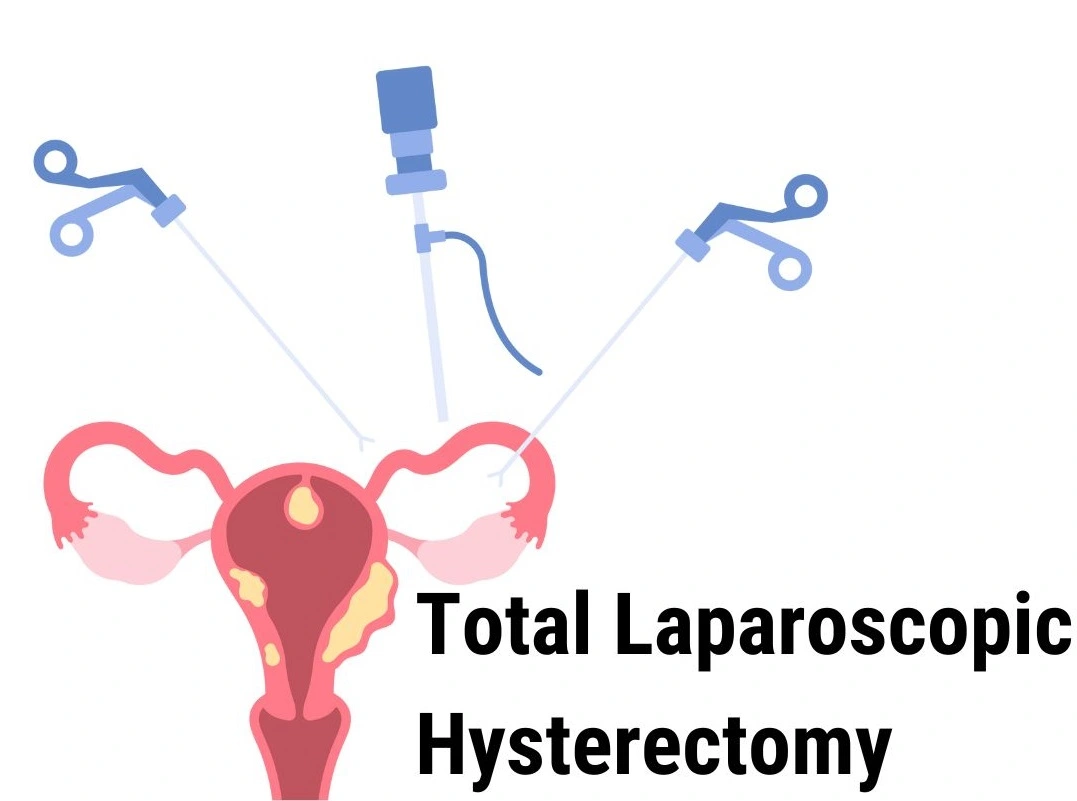
TLH
Small incisions and a laparoscopy to remove the uterus.

LAVH
Combines laparoscopic & vaginal techniques for minimally invasive.

Advanced Prenatal Checkups in Mathura
Pregnancy assessments, which are important medical evaluations, involve close monitoring of both the developing baby and the expectant mother’s health at various points. During those visits, an obstetrician or gynecologist may also often conduct certain tests and examinations to make sure the pregnant woman is healthy.
Prenatal care sometimes involves physical checks, blood, urine, and ultrasound scans to look for any abnormalities or ability difficulties. These exams are scheduled based on the stage of pregnancy, with later visits being more frequent. Prenatal tests enable expectant mothers not only answers to questions but also recommendations on exercise, diet plans, and many aspects of prenatal care, as well as equipping them for success.

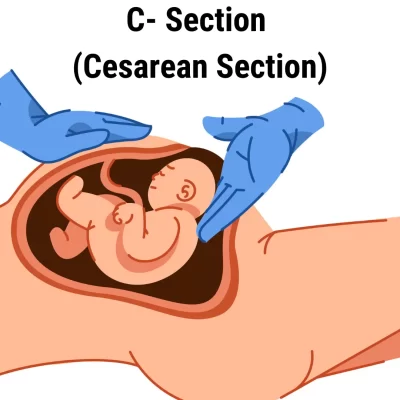
C- Section: A Guide to Cesarean Deliveries
A cesarean section, commonly commonly known as a C-section or cesarean delivery, is a surgical operation in which the mother’s uterus and diaphragm are cut open to deliver the baby. When a vaginal birth turns out to be unsafe for the woman, the child, or both, it is carried out. For a safe and expert C-section delivery in Mathura, BL Tiwari Memorial Hospital offers top-notch care.
MTP (Medical Termination of Pregnancy)
Abortion, also known as Medical Termination of Pregnancy (MTP), is a medical treatment used for terminating a pregnancy before the unborn baby reaches the fertile stage. It is a vital element of the care for female reproductive health that deals with serious hidden scientific, and ethical issues. Girls are given the opportunity to make informed decisions about their bodies, fitness, and futures through MTP.


DNC (Don’t Needle Comfort)
An innovative method of treating pain called “Don’t Needle Comfort” seeks to do it without the requirement of invasive procedures or needles. In order to treat the underlying cause of pain and encourage natural healing, this holistic approach includes a variety of modalities, including massage, acupressure, and herbal therapies. The program provides a secure and reliable substitute for conventional pain treatment techniques, and it is made to be accessible to people of all ages and backgrounds.
Don’t Needle Comfort encourages people to take charge of their own health and manage their pain without resorting to potentially dangerous drugs or surgical procedures. This is achieved by emphasizing the body’s natural capacity to heal itself. Numerous people have found chronic pain relief and overall quality of life improvement with Don’t Needle Comfort’s emphasis on natural therapies and individualized care.
Tubectomy
A tubectomy is a permanent start manipulation procedure that is also referred to as a tubal ligation. The sperm must reach the eggs for the process of fertilization in order for a pregnant being to manifest. In order to prevent sperm from accessing the eggs, the fallopian tubes are cut, tied, or sealed during this surgical procedure. Up until now, safe and successful birth control treatments have included exclusive variants of tubectomy, which are seen to be one of the most effective starting control strategies.It is your private decision to start manipulating, no matter whether you decide to have children at all or none at all. Delivery methods are more popular than ever, but choosing the appropriate one is a crucial decision that requires careful planning. Among the reasons you may be considering a tubectomy are population control, limited household sizes, and rising costs. One type of initial manipulation procedure is the tubectomy.
If you’re making plans to get your tubes tied, it is vital to recognise all about tubectomy. Let’s understand what tubectomy is, its method, advantages and possibly facet consequences.
Tubal sterilization is another name for the tubectomy procedure. Recall that the tubal ligation procedure can be extremely painful, expensive, and challenging to reverse. A lot of people have it done following a C-phase (Cesarean transfer) or any other stomach surgery.
For top tubectomy care in Mathura, visit BL Tiwari Memorial Hospital, where expert and compassionate treatment is provided.
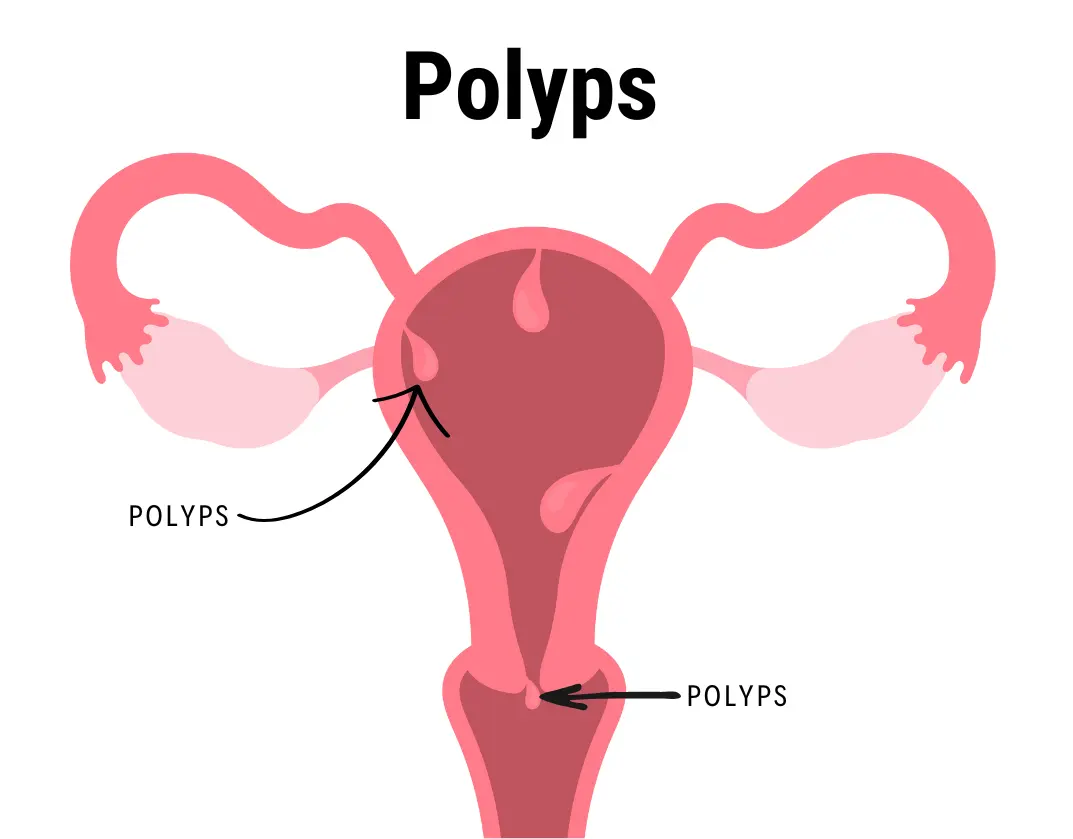
Polyps
Polyps seek advice from anomalous tissue growths that often expand on the tissue layers lining various organs, mainly the belly, the womb, intestines, and nasal passages. From miniature, flat lesions to bigger, stalk-like paperwork that resembles tiny mushrooms, these growths can vary significantly in length and appearance. Some polyps can also result in symptoms like bleeding, ache, or blockage regardless of wherein they are, although most polyps are innocent and asymptomatic. Oral polyps, as an instance, can result in rectal bleeding or altered bowel conduct, even as nasal polyps can motivate persistent congestion and sinus infections. Uniquely, for people with a family history of polyps or specific genetic problems, routine screening and tracking are vital in view that a few polyps have the ability to develop into cancer.
Chronic infection, lifestyle selections, and genetic predispositions are some of the variables that affect the development of polyps. Particularly in the gastrointestinal system, inflammatory diseases, inclusive of Crohn’s ailment and ulcerative colitis, would possibly enhance the threat of polyp improvement. Their advent can also be attributed to way of life elements like smoking, heavy alcohol intake, and a diet excessive in fat and poor in fiber. In order to forestall possible malignant transformation, polyps have to be determined and removed. For the reason of finding and doing away with polyps within the colon, colonoscopy is aneducing the danger of cancer and controlling the signs associated with polyps want early detection and motion. often used diagnostic and healing technique. For polyps positioned some other place in the frame, imaging assessments and biopsies may be hired. For expert care for polyps in Mathura, visit BL Tiwari Memorial Hospital.
High-Risk Pregnancy
Conditions that could endanger the mother’s, the unborn toddler’s, or each’s fitness are what outline a high-risk pregnancy. Pre-existing clinical problems which include diabetes, hypertension, or autoimmune illnesses are only a few of the variables that would make a pregnancy excessive-threat. Pregnancies in girls below 17 or over 35 are regularly considered a better threat due to their age, that is every other important determinant. Risks also can be multiplied with the aid of lifestyle picks like consuming alcohol, smoking, and receiving insufficient prenatal care. Other contributory elements include hereditary issues, a history of pregnancy troubles, and multiple pregnancies (twins, triplets, and so on.). For any difficulties to be safely controlled, those pregnancies require professional hospital treatment and closer monitoring.
To get the greatest consequences for mother and infant, handling a high-hazard pregnancy requires a multidisciplinary approach. It is vital to have ordinary prenatal appointments, which generally consist of extra common take-a-look-ups, ultrasounds, and specialized trying out to assess the mom’s fitness and the infant’s development. Healthcare professionals may advise remedy, lifestyle changes, or different interventions to deal with pre-existing situations and decrease associated dangers. Bed rest or hospitalization may be required in a few conditions to shield the fitness of the mom and fetus. The anticipating woman can better understand her scenario and the actions she can take to save you difficulties through receiving schooling and aid, which are also critical. Navigating the problems of a high-chance being pregnant and ensuring a Normal Delivery depend closely on early detection and powerful control.

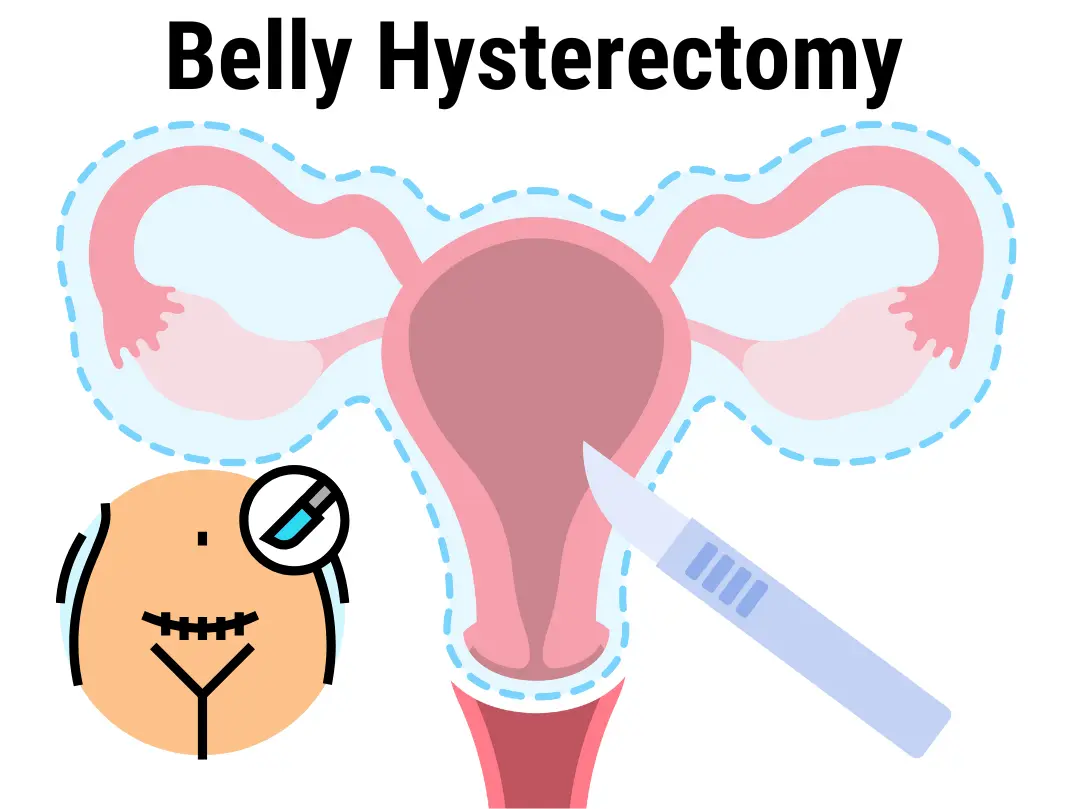
Belly Hysterectomy
A cut made in the lower stomach allows the surgeon to remove the uterus during a belly hysterectomy, also known as an abdominal hysterectomy. The technique is frequently implemented in situations involving vaginal expansion or where additional genital tissue, such as the fallopian cysts or ovarian cysts require to be eliminated. Standard the anesthesia is typically used to make sure that the patient remains asleep and free of pain during the surgical operation. The cut can be horizontal, placed next to the trunks line, or vertical, extending from just below the navel to just over the bone that supports the pubic bone. Due to the more intrusive nature of the treatment, recovery from an abdominal hysterectomy typically takes longer than that of other hysterectomies, including vaginal or laparoscopic hysterectomies.
Many medical conditions, such as endometriosis, fibroids in the uterine cavity, chronic pelvic discomfort, and the majority of ovarian, cervical area, or uterine tumors, may require this type of hysterectomy. Patients can also suffer from an array of sensations during the operation, which includes as stiffness, swelling, and restricted motion, which may persist for several weeks. To stay away from problems such as viruses or blood clots, patients need to strictly adhere to their the doctor’s after surgery treatment directions. To demonstrate healing and address any concerns that may arise during the recovery process, follow-up meetings on a regular basis are essential.
Vaginal Hysterectomy
Vaginal Hysterectomy Surgery in Mathura is a surgical procedure where the inguinal canal is opened for the removal of the abdominal cavity. Because the process does not require making an extensive cut in the digestive tract wall, it is considered as less painful than a belly hysterectomy. During the surgical process, the physician separates the womb from the blood arterial walls and ligaments that support it, as well as from the fallopian tubes, ovary, and upper cervix. After that, the uterus is removed through the vaginal canal. Although it usually involves a shorter healing time and a lower risk of consequences than other surgical methods, this type of hysterectomy is preferred for certain healthy conditions, such as uterine prolapse, excessive monthly bleeding, fibroids, or chronic pelvic discomfort.
After a vaginal hysterectomy, patients usually notice substantially fewer pain post operation, shorter hospital stays, and quicker recovery periods. But not each individual patient is a good fit for this system at this point. The shape and size of the womb, the amount of tissue scarred from previous operations and the deeper health issue needed for the hysterectomy are some of the variables that could affect the choice. Along with infection, bleeding, and harm done to right next organs, there are risks related to ability, as with any type of surgery. Patients should have a conversation with their healthcare provider about which type of hysterectomy is best for their particular scientific needs.
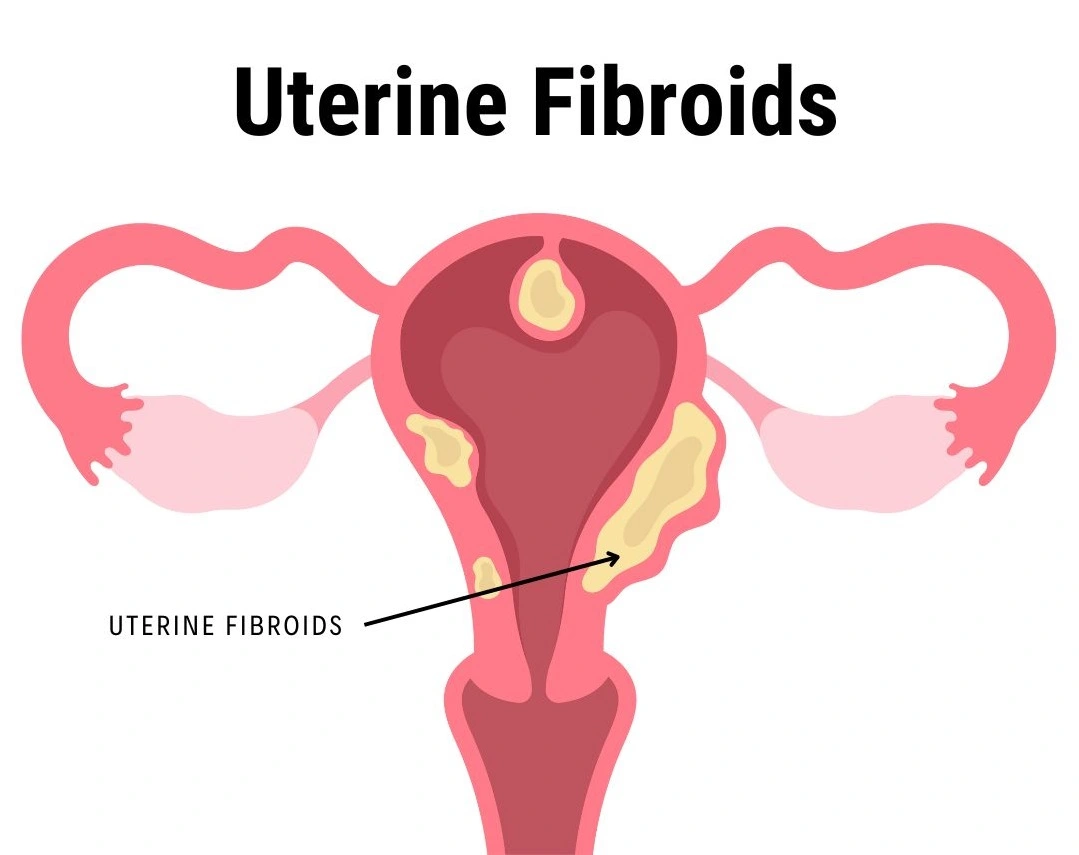
Uterine Fibroids
Non-cancerous growths that expand within or close to the female reproductive tract are commonly referred to as uterine fibroids, leiomyomas, or myomas. These benign tumors can vary in size from microscopic to huge hundreds, that are capable of bending and enlarging the uterus. They are formed out of connective tissue with fibers and easy cells of muscles. Genetic traits that are boom elements, and hormonal deficiencies (particularly with regard to progesterone and estrogen) are thought to play a significant part in the development of fibroids, even though the precise purpose of them isn’t always completely known. Women who are fertile will frequently get fibroids; research suggests that by the time they are 50 years old, 70–80% of women will have developed them, however many will remain asymptomatic.
The amount of tissue, spread, and positioning of fibroids located within the uterus affect their signs and symptoms. Continued cycles, pain in the pelvis or tension, bleeding during the menstrual cycle, frequent urination, and problems during delivery and pregnancy are typical symptoms. Infertility sometimes comes from fibroids. magnetic resonance imaging (MRI ultrasounds, and pelvic exams are frequently utilized whenever possible with different types of imaging to make the diagnosis. Depending on the severity of the symptoms, there may be non-invasive options such uterine artery embolization, symptom-controlling drugs, or surgical procedures like hysterectomy or myomectomy (removal of the uterus) to treat the condition. BL Tiwari Memorial Hospital provides excellent care for a professional and safe Uterine Fibroids Treatment in Mathura.
TLH (Total Laparoscopic Hysterectomy)
A minimally harmful surgical technique called a total laparoscopic hysterectomy (TLH) is utilized for the removal the female reproductive organ. During this method, tiny cuts are made inside the tummy that allow for specific instruments for surgery and a laparoscope—a lighted, thin tube with a digital camera—are inserted. By applying a laparoscope, medical professionals can observe their digestive tract on a screen, providing a magnified picture that helps them do accurate surgical techniques. The uterus is then removed through the vagina or one of the tiny incisions after being severed from the surrounding tissues and blood vessels. The TLH procedure is often preferred over traditional open surgery due to the associated benefits, which include decreased pain following surgery, shortened hospital stays, and expedited recovery periods.
Numerous gynecological circumstances, such as endometriosis, persistent pelvic pain, irregular bleeding during menstruation, fibroids in the womb, and some gynecologic cancer, belong to the potential causes for TLH. The choice of whether to conduct TLH is based on a number of factors including the health status of the patient, the shape and size of the uterus, and the physician’s level of expertise. Like any surgical approach, total ligament herniation (TLH) includes some risk, such as hemorrhaging, infection, and injury to nearby organs; however, the risks usually smaller than those associated with open surgery. Thanks to developments in laparoscopic technology and techniques, TLH has become a safe and effective option for many women who need hysterectomy, providing improved outcomes and a higher quality of life after surgery.
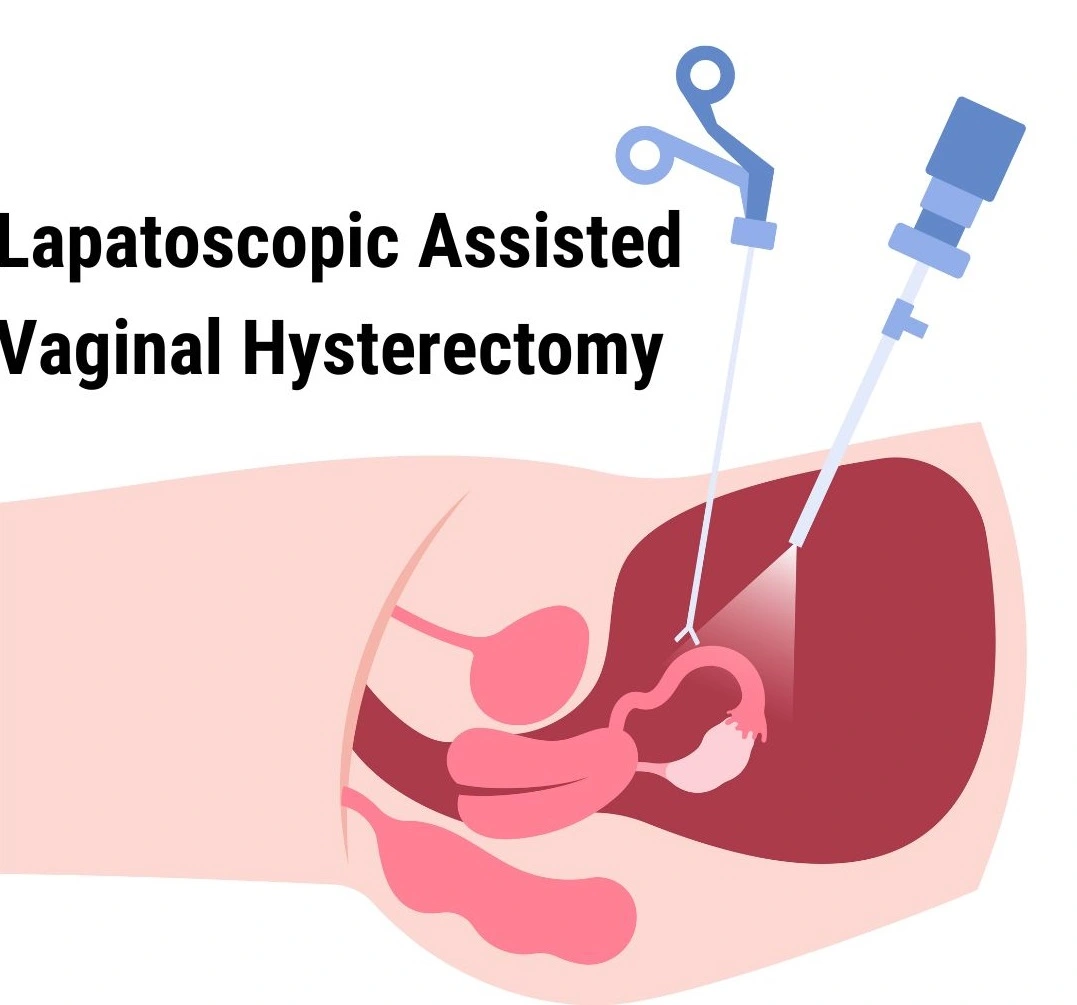
LAVH (Lapatoscopic Assisted Vaginal Hysterectomy)
A very minimally invasive treatment called laparoscopic assisted vaginal hysterectomy (LAVH) is done for the removal the abdominal cavity. It integrates urinary surgical intervention to remove the uterus through the genital canal with endoscopic methods, which require making tiny cuts in the belly and using a video camera and specific tools to visualize and aid with the surgical operation. When various therapies have failed, this operation is frequently used for diseases such as endometriosis, uterine fibroids, irregular uterine flow, and persistent discomfort in the pelvis. Comparing to a standard pelvic hysterectomy, laparoscopic and vaginal techniques are combined in LAVH to provide the benefits of a less intrusive treatment, as well as reduced pain following surgery, shortened hospital stays, and quicker recovery times.
During a LAVH, the surgeon makes numerous small incisions in the stomach to insert the laparoscope and different gadgets. These tools permit for unique dissection and management of the blood vessels and ligaments surrounding the uterus. Once the uterus is detached, it’s miles removed through the vaginal canal. This method permits for better visualization and access to pelvic structures, that may enhance surgical precision and protection. Patients undergoing LAVH commonly revel in fewer complications and a quicker return to regular activities in comparison to the ones present process traditional open surgical operation. As with any surgery, however, LAVH carries ability risks, together with infection, bleeding, or harm to surrounding organs, and it is essential for patients to speak about these risks with their healthcare company.



